
Three conversations this week showed how easy it is to get seduced into doing the wrong thing. All of these showed that if primary care focuses its change effort on fad or ill informed policy it will just make things worse. We have to take an evidence based view.
These were the conversations:
- Helen Carr, Local Care Direct West Yorkshire about who is accessing out of hours and its young people
- Ollie Hart, GP from Sheffield on twitter about Marmot 2
- The Steering Group of the RSA Future of Health and Care the topic is in the group title!
Primary Care for Young People
You have seen this slide before – where we show that young people aged 7-24 are not accessing GP appointments.

What Helen told me was shocking. She said that across West Yorkshire 30% of the out of hours demand was for young people aged 16 and under.
Earlier in the week I’d been contacted by a network of PCNs who had decided to tackle the issue primary care for young people – which is really great. They were going to go to schools and tell them about social prescribing and the services they were offering. The data above tells us that walking into a GP practice is not what young people want or need. I suggested two things to the PCN Network to think about:
- Be clear that you are prepared to spend the allocation per head you receive for these young people on meeting their needs. It may well be that you need to offer something quite different from traditional services.
- Yes go out to schools but be prepared to listen first – what does the school know about the health needs of young people in their care (when I was a school governor the pastoral team were overwhelmed with young people with anxiety, self-harming, drugs, poor family life..); and then listen to the young people themselves – what is it that helps them live a good and healthy life? Where do they go for help? What would work for them?
Marmot, Poverty and Primary Care
When you read my blogs on people who attend frequently in Primary Care you will see that there are 3 main issues:
- People who need continuity of care
- People who need a multidisciplinary team to meet their complex needs
- People who are struggling with life – not just loneliness, but poverty.
My vlog (at the bottom of this blog) on working with general practice and their communities, shows that when you ask communities they say that to live a good and healthy life firstly people need shelter, stable finances, family and friends, meaningful lives and work etc. But the Marmot Review 10 years on shows us how these basic needs are not being met and are undermining people’s health:
- “For part of the decade 2010-2020 life expectancy actually fell in the most deprived communities outside London for women and in some regions for men. For men and women everywhere the time spent in poor health is increasing.
- Put simply, if health has stopped improving it is a sign that society has stopped improving.
- The fact that austerity was followed by failure of health to improve and widening health inequalities does not prove that the one caused the other. That said, the link is entirely plausible, given what has happened to the determinants of health.” (p5) And this is the graph that demonstrates this (p10)

General Practice is experiencing an increase in demand directly related to people’s social conditions. No amount of social prescribing and extended hours will solve this problem – it needs to be solved at source. I don’t know how many appointments are for poverty-created health needs, but we need to find out. As I said at the RCGP conference – primary care has to understand need so it can push back against policies that are sticking plasters not problem solvers. Once we know this we can work with local government, our political representatives and the public to help people. I would argue GPs have a professional duty to do so.
Another key issue here is the disproportionate impact for the minority ethnic population , and that leads me to the last conversation
Modelling the future to reinforce the status quo
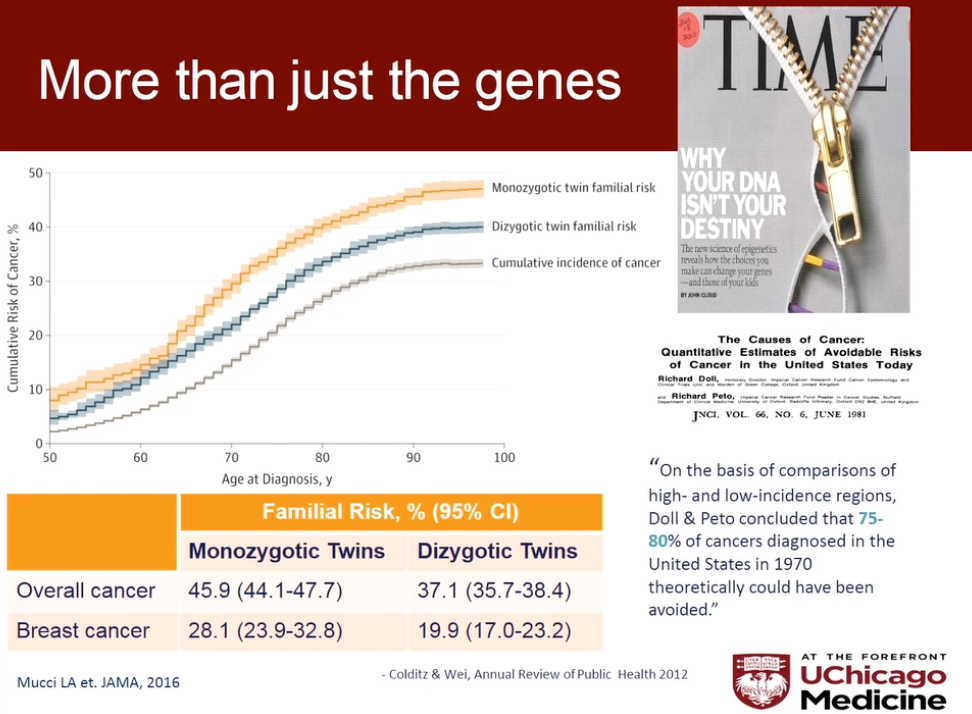
I was at a meeting of the Advisory Group for the RSA’s Future of Health and Care work. One area that is generating a lot of attention is genome sequencing and the ability to predict people’s health almost from birth. However a few weeks ago I’d chaired a cancer conference for Inspire2Live (a brilliant organisation that brings the best of science, clinical knowledge and citizen leadership together) rather cleverly called “Evidence, Arrogance, Ignorance, Eminence’ – which rather sums up the NHS dilemma. These presentations got to the heart of the issues:
- Bob Weinberg (Whitehead Boston Institute) – the more we investigate cancer the more it outsmarts us – the science is telling us (a) we have to stop over treating and be more nuanced in care and (b) prevention is more effective and for lung cancer the only solution is to reduce incidence. Presentation . Have a look at the impact of education level (thank you Bob)

- Olufunmilayo Olopade (University of Chicago) – the research on breast cancer is primarily from studies of white western women and it doesn’t translate to ethnic minority groups. Presentation
- Patrick Connor (pharmaceutical company AstraZeneca) – whist science has almost eliminated some cancers, we need to take a differnt tack with others – improving quality of life, and working on prevention already working on new grants for collaboration. Presentation
No amount of genome sequencing is going to help if (a) our data for determining solutions does note reflect the ethnic mix of our population and (b) we don’t address the critical issues of living healthy lives …. we are back to Marmot. The future of health and care is in living well not treating disease accelerated by poor social norms (poverty, investment in education…).

Hi Becky
Please could you email me and advise which PCN has engaged Health and Wellbeing Coaches into Schools. You mention in your blogs
We are looking at doing this, we have engaged one Acadamy, A Mental Health Charity and a CCG Mental Health Lead
Learning from another PCN Model would be invaluable
Thanks
Dan Reid
CD Solihull Rural PCN
LikeLike